Dr Stephen Cole
Obstetrician & Specialist in Maternal-Fetal Medicine
MBBS, FRANZCOG, CMFM, DDU
About Me
I am an obstetrician practicing in Melbourne, Victoria. In addition to standard obstetric training, I also have further specialist training, qualifications and experience in caring for women with the highest risk and most complex pregnancies.So whether you are anticipating a straightforward pregnancy or come into your pregnancy with concerns about important risks, I am able to provide the expert, personalised care you require.
Find out more
Your First Visit
Your first visit is a very important visit for your pregnancy. It is ideal though not essential that both you and your partner attend this visit.During this visit we will discuss your helath and your pregnancy in depth, I will ble to answer any and all questions or concerns, what to expect and how to be the most prepared and ready for the amazing journey ahead.
How can I help you?
Let's discuss your pregnancy.
If you have any questions or enquiries please feel free to contact us on the following details provided below or alternatively you can complete our online enquiry form also located below and we will get back to you as soon as possible...
Let’s Talk About COVID-19 and Pregnancy
Welcome to my ‘Let’s Talk’ Blog. The idea behind ‘Let’s Talk’ is to answer some of the more common questions people ask about pregnancy and pregnancy care. ‘Let’s Talk’ also aims to provide information on some of the more interesting or challenging issues that women who are pregnant or planning for pregnancy may face.
So today’s blog is focussing on the hottest topic on the planet at the moment – COVID-19, and in particular, what pregnant women need to know about it.
But first – a disclaimer. COVID-19 is a very newly discovered infection. New information is being uncovered every day, and our understanding of the disease will develop along with that new information. I will attempt to keep this blog up to date, but new developments may not be captured immediately. This blog is for general information only. It should not be taken as medical advice. If you are concerned about your health, you should seek expert medical advice.
Pregnancy is an incredibly exciting time for most women, but it is also a time of considerable anxiety and stress. This article is written to help you make sense of what is going on around you and minimise the COVID-19 related stress that so many pregnant women are feeling at the moment.
What is COVID-19?
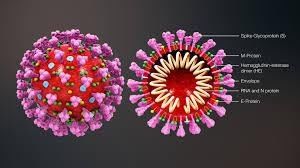
COVID-19 is the name of the disease caused by a new type of coronavirus. That coronavirus is known as SARS-CoV-2. Coronaviruses are a family of viruses named for their distinctive appearance – in particular their “crown of thorns”.
Coronaviruses cause infections in the airways and lungs. They are responsible for both minor illnesses like the common cold, and more serious infections such as Sudden Acute Respiratory Syndrome (SARS). The virus now named SARS-CoV-2 was first detected in Wuhan, China in December 2019. It is not clear where this new virus came from. While there is speculation that it crossed over from animals to humans, there is currently no confirmed explanation.
Infection with the coronavirus SARS-CoV-2 causes the illness COVID-19. COVID-19 can cause a range of different symptoms, including fever, cough, sore throat, runny nose, aches and pains, tiredness, loss of taste or smell, and breathing difficulties.
The majority of people infected with COVID-19 have quite mild symptoms, and some may have no symptoms at all. Approximately 15% of people infected experience symptoms (usually breathing difficulty) that require them to go to hospital. 5% become so unwell that they require admission to an Intensive Care Unit (ICU).
In Australia the death rate for COVID-19 is just over 1%. In some other countries it has been higher – up to 4-5%. Whilst older patients are most likely to suffer the more serious consequences of COVID-19, younger people may also be severely affected.
Who needs testing?
If you have any of the symptoms above, or if you think you may have been in contact with someone who has COVD-19, you should be tested. Some people may also be asked by the Department of Health to get tested. This request is usually only made when the Department of Health has reason to believe you might have come into contact with someone with a confirmed case of COVID-19. If you have been tested you will need to check with your doctor as to whether you are required to self-isolate until the result of your test is known.
COVID-19 and Pregnancy
The impact of COVID-19 on pregnancy is not completely clear. More data is being collected every day, and the research is going to tell us more about the relationship between COVID-19 and pregnancy. However, there are a few comments that can be made.
Throughout a pregnancy, women experience changes in their immune system that can make them more susceptible to infections and illnesses than they would otherwise be. They can find themselves experiencing more intense symptoms. This is certainly true for Influenza (AKA: ’The Flu’), and other coronavirus infections.
Thankfully, this doesn’t seem to be the case for COVID-19 – at least so far. Around the world there are reports of pregnant women becoming seriously unwell, and there have also been some reports of pregnant women dying. But these are rare cases, and don’t seem to occur at a frequency higher than in non-pregnant women and in men.
But while pregnant women may not be at higher risk of the serious consequences of COVID-19; they should, like all of us, practice appropriate personal hygiene and social distancing measures to minimise the chance of infection.
Probably the area of most concern is the risk of COVID-19 infection leading to premature / preterm birth. In the published reports so far, the rates of preterm birth seem quite high. What is less clear is what the cause of those preterm births are. There may well be an increase in preterm birth caused by the virus. But it also seems to be the case that many reported preterm births are due to doctors choosing to deliver infected patients early. It will take a while to sort these issues out, as we collect more information on larger numbers of infected pregnant women.
Another area that concerns parents is the risk of birth defects. At this stage we have no information about this. Birth defects caused by viruses tend to occur when infection happens in the first few weeks of pregnancy. Because COVID-19 was first detected only in December 2019, women who were in early pregnancy when they were found to be infected have not given birth yet. So we don’t have any information about their babies. Unfortunately it isn’t possible to make any meaningful comment on this issue at the moment.
COVID-19 and Newborn Babies
It is unclear whether COVID-19 can cross the placenta and cause infection in babies in the womb. A small number of cases where this may have occurred have been reported, but there are questions about the timing of testing, etc. Certainly it seems that in the majority of cases fetal infection with COVID-19 (i.e. infection in the womb) does not occur.
Another area of concern is breastfeeding. So far, from all of the studies that have looked for SARS-CoV-2 in breast milk from infected mothers, it seems that the virus isn’t carried in breast milk. However, it is important to remember that breastfeeding is a time of close, prolonged contact between mothers and babies. This physical contact probably poses more of a risk than any risk of transmission via breast milk.
Changes In Pregnancy Care Due To COVID-19
Doctors, hospitals and health departments have made changes to the way they provide care to pregnant women throughout this crisis. These changes are designed to protect women and babies, and also to protect health care workers. The exact changes that you may experience will vary from hospital to hospital. I recommend that you check in with your doctor or hospital to find out more about the specific changes they have made.
There is one change that is uniform across the country; and it is expected of you before you arrive at a hospital or clinic. Anyone experiencing symptoms that might be COVID-19 related must notify their doctor or hospital before attending an appointment. This is expected even of those presenting with only mild symptoms. See above, or consult the DHHS for a list of possible symptoms.
To give you a better idea of some other measures that have been brought in, here are some examples of the changes that some hospitals and private practices have put in place:
- Some visits may be conducted by telehealth (telephone, Zoom, etc)
- All hospitals and many clinics require that your temperature is checked before you are allowed to enter the building
- Some clinics may require you to use hand sanitiser, gloves, or masks, and may aim to keep visits shorter
- You may be asked to wait outside or in your car if you are early or the doctor is running late, to minimise the number of people in the waiting room
- Some clinics may not allow you to have anyone else with you when you attend for visits, scans, etc
- Some tests may change (eg the test for diabetes in pregnancy previously required women to sit in the waiting room for 2 hours. This has been changed in some centres)
- Antenatal classes / birthing education classes have either been cancelled, set up as online education tools, or are being run by Zoom / Google Meets / etc – check with your hospital
- Staff in the birthing suite may be wearing masks and other personal protective equipment (PPE)
- Many hospitals are not allowing any visitors other than the woman’s partner / support person. This has understandably caused some disappointment, as visits from family and friends to meet the new baby are a highlight for many new parents
- Stays in hospital after birth may be shorter
- Midwife / Maternal-Child Health Nurse home visiting programs may be suspended or modified.
What If I Have COVID-19 In Pregnancy?
Most women who have COVID-19 during pregnancy will experience minor symptoms, and will be expected to make a full recovery. Only a fraction of the number of women who contract the illness during their pregnancy will experience more serious symptoms.
If you contract COVID-19, you will be required to self-isolate until you are advised that you have cleared the infection and are safe to move around in the community again. You’ll need to contact your doctor or hospital to notify them of your circumstances, and to discuss arrangements for your pregnancy care. You will still need to have check-ups, etc, but these may need to be modified to suit your circumstances.
If you have COVID-19, or have symptoms that suggest an infection when you come into hospital to have your baby, there will likely be some changes to the way you receive care. These changes will be required to reduce the risk of infection to the staff caring for you, and the risk to other patients in the hospital. You will need to discuss these changes in detail with your hospital and your doctor.
COVID-19 and Breastfeeding
If you have COVID-19 and you want to breastfeed, you will still be able to do so. At the moment there is no evidence that COVID-19 is transmitted via breast milk. The benefits of breastfeeding still far outweigh the risks. Due to the close contact you will have with your baby during this time, you should wear a mask, and practice good hand hygiene to reduce the risk of passing on the infection to your baby. Some people may also choose to wear gloves.
COVID-19 and Pregnancy Resources:
https://www.dhhs.vic.gov.au/coronavirus
https://www.health.gov.au/news/health-alerts/novel-coronavirus-2019-ncov-health-alert
https://ranzcog.edu.au/statements-guidelines/covid-19-statement/information-for-pregnant-women
https://www.rcog.org.uk/en/guidelines-research-services/guidelines/coronavirus-pregnancy/covid-19-virus-infection-and-pregnancy/
https://www.centreforperinatalpsychology.com.au/resources-covid-19/
Dr Stephen Cole, Specialist Obstetrician
Since 2001, I have been an obstetrician in East Melbourne providing care for women with both low and high-risk pregnancies. As an MFM (Maternal-Fetal Medicine) specialist, I see women with a wide range of pregnancy situations. The odds are that your pregnancy will be low risk and go smoothly; however, should complications arise, you can be confident that I am well equipped to handle even the most high-risk pregnancies and unexpected complications. Private hospitals where I work include Epworth Freemasons, Frances Perry House, and St. Vincent’s Private. I strive to provide woman-centred care, and I am supportive of my patients’ choices. Many obstetricians claim to be “high risk” specialists, but only MFM specialists have undergone the training and assessment needed to manage all pregnancies, from the simplest through the most complex. Please contact me with any questions or concerns on (03) 9495 6411 or via my online contact form.